Are implants poised to become patients top choice when faced with tooth loss?
While it's certainly true that third-party coverage—or the lack thereof—may be the greatest obstacle that keeps patients from opting for dental implants, the dental profession has done its part to ensure that the products and techniques are in place to take implant dentistry to the next level. The quality, range, and efficacy of today's implants are the result of continuous research and development that has arguably been the most energetic and productive in the history of dentistry.
Florida oral and maxillofacial surgeon David Feinerman, DMD, MD, shared his observations about what patients are demanding from implant treatment. “Expectations include the desire for implant treatment that is relatively noninvasive, painless, low cost (or at least less costly), quick overall, and with fewer treatment phases, as well as for immediate restorative care,” Dr. Feinerman said.
Improvements in hardware and protocol have certainly been focused on all these patient concerns, and as a result, the evolution of dental implantology can be outlined with the help of a handful of key buzzwords:
Anatomy. Osseointegration. Biocompatibility. Digitization.
Anatomy
One-size-fits-all described the design of pre-Brånemark attempts at "implants" and even early cylindrical designs. Little thought was given to shape or size. The first attempts at designing implants that accommodate conditions in the mouth centered only on varying the implant length. Variable circumferences and tapering soon followed. Currently, the thousands of size and shape variations available address the individual anatomical challenges of most patients, from narrow interdental spaces to inadequate or excessive alveolar bone.
Solutions like Dentatus' Anew Narrow Body implants are specifically designed to accommodate interdental spaces and divergent angles as narrow as 3.5 mm. These narrow-diamater implants provide solutions to the solutionless, as they are ideal for patients who lack the time, finances, or bone structure required for conventional implants. The screwretained prosthetic system is immediately loaded and easily disassembled without tapping, which prevents micromovement.
Dr. Adam Koppelman, who offers implant dentistry at his practice in New York City, NY, feels that patients shouldn't be condemned to life with a removable appliance and, on the same note, that narrow-diameter implants are an asset to any implant armamentarium. "By offering narrowdiameter implants in our practice, we've turned impossibilities into realities for our patients," he shared. "We offer them something they've been told most of their lives couldn't be done; we offer them hope, and hope is pretty powerful."
Osseointegration
Two main developments have dramatically simplified and increased the predictability of osseointegration. First, different types of grafting materials, along with advancements in delivery and placement procedures, have made dental implants a viable option for patients who previously were not good candidates because of compromised bone quantity or quality. “I believe progress in the area of bone growth—particularly making healing faster and more predictable with the use of bone-stimulating factors—will be the most significant improvement in dental implantology in the near future,” observed prosthodontist Dr. Randolph Resnik of the Misch International Implant Institute.
Secondly, most implants now feature some type of surface treatment and/or coating to facilitate osseointegration. Specifically, implants have almost universally moved from smoothsurfaced to having roughened surfaces that maximize contact area. Additionally, specialized coatings—ranging from bisphosphonate and fluoride to proprietary formulations such as Straumann's SLActive—now are available to enhance and speed integration and improve longevity.
A good example of this surface treatment at work can be found in Nobel Biocare's NobelActive implants, which feature oxidized TiUnite surfaces that help maintain stability during healing. A moderately rough and thickened titanium oxide layer provides high crystallinity and osteoconductive properties that lead to faster bone formation, and ultimately, greater long-term success.
Florida oral and maxillofacial surgeon David Feinerman, DMD, MD, shared his observations about what patients are demanding from implant treatment. “Expectations include the desire for implant treatment that is relatively noninvasive, painless, low cost (or at least less costly), quick overall, and with fewer treatment phases, as well as for immediate restorative care,” Dr. Feinerman said.
Improvements in hardware and protocol have certainly been focused on all these patient concerns, and as a result, the evolution of dental implantology can be outlined with the help of a handful of key buzzwords:
Anatomy. Osseointegration. Biocompatibility. Digitization.
Anatomy
One-size-fits-all described the design of pre-Brånemark attempts at "implants" and even early cylindrical designs. Little thought was given to shape or size. The first attempts at designing implants that accommodate conditions in the mouth centered only on varying the implant length. Variable circumferences and tapering soon followed. Currently, the thousands of size and shape variations available address the individual anatomical challenges of most patients, from narrow interdental spaces to inadequate or excessive alveolar bone.
Solutions like Dentatus' Anew Narrow Body implants are specifically designed to accommodate interdental spaces and divergent angles as narrow as 3.5 mm. These narrow-diamater implants provide solutions to the solutionless, as they are ideal for patients who lack the time, finances, or bone structure required for conventional implants. The screwretained prosthetic system is immediately loaded and easily disassembled without tapping, which prevents micromovement.
Dr. Adam Koppelman, who offers implant dentistry at his practice in New York City, NY, feels that patients shouldn't be condemned to life with a removable appliance and, on the same note, that narrow-diameter implants are an asset to any implant armamentarium. "By offering narrowdiameter implants in our practice, we've turned impossibilities into realities for our patients," he shared. "We offer them something they've been told most of their lives couldn't be done; we offer them hope, and hope is pretty powerful."
Osseointegration
Two main developments have dramatically simplified and increased the predictability of osseointegration. First, different types of grafting materials, along with advancements in delivery and placement procedures, have made dental implants a viable option for patients who previously were not good candidates because of compromised bone quantity or quality. “I believe progress in the area of bone growth—particularly making healing faster and more predictable with the use of bone-stimulating factors—will be the most significant improvement in dental implantology in the near future,” observed prosthodontist Dr. Randolph Resnik of the Misch International Implant Institute.
Secondly, most implants now feature some type of surface treatment and/or coating to facilitate osseointegration. Specifically, implants have almost universally moved from smoothsurfaced to having roughened surfaces that maximize contact area. Additionally, specialized coatings—ranging from bisphosphonate and fluoride to proprietary formulations such as Straumann's SLActive—now are available to enhance and speed integration and improve longevity.
A good example of this surface treatment at work can be found in Nobel Biocare's NobelActive implants, which feature oxidized TiUnite surfaces that help maintain stability during healing. A moderately rough and thickened titanium oxide layer provides high crystallinity and osteoconductive properties that lead to faster bone formation, and ultimately, greater long-term success.
THE INCREDIBLY SHRINKING IMPLANT
With expanding applications and proven efficacy, look for these shorter and narrower implants to continue their popularity.
When the Bicon SHORT Implants system was introduced in 1985, their 8.0 mm length was considered quite short compared to the more common 12- to 14-mm length at the time. Since then, the natural progression of Bicon's design philosophy has resulted in 5.0-mm and 6.0-mm SHORT Implants, which maximize implant placement possibilities and minimize the need for grafting procedures.
Dentsply Sirona's AstraTech family features the OsseoSpeed EV line, with implants available in a versatile range of shapes, diameters, and lengths—6 mm to 17 mm—for all indications, including situations with limited space and/or bone quantity. For conical implants, the body portion is 0.6 mm narrower.
Dentatus' Anew Narrow Body implants are ideal for patients with insufficient bone width, limited interdental space, or converging roots. Designed for use in small interdental spaces for fixed restorations, Anew implants come in diameters of 1.8, 2.2, and 2.4 mm. A nonhygroscopic screw cap allows for implants to be monitored, altered, and easily adapted to a permanent restoration.
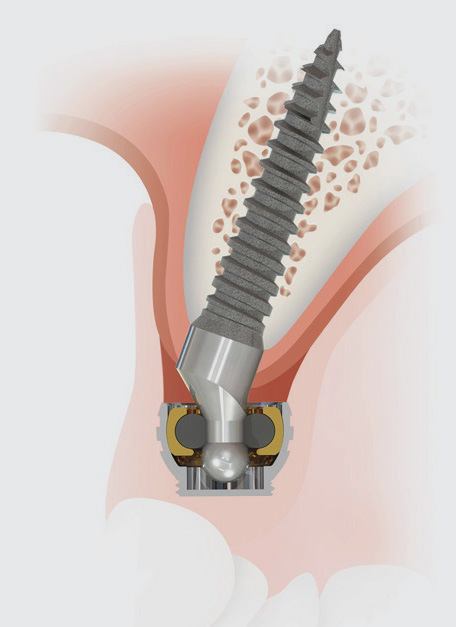
For patients whose anatomical limitations prevent them from receiving treatment with standard-diameter implants, the SATURNO Narrow Diameter Implant from Zest Dental Solutions features a 1-piece design with a pivoting O-Ball connection that provides maximum resiliency while maintaining a minimized profile. The implants—available in a straight or a 20° angle for addressing common challenges in the maxillary ridge—come in diameters of 2.0, 2.4, or 2.9 mm and lengths of 10, 12, or 14 mm.
With expanding applications and proven efficacy, look for these shorter and narrower implants to continue their popularity.
When the Bicon SHORT Implants system was introduced in 1985, their 8.0 mm length was considered quite short compared to the more common 12- to 14-mm length at the time. Since then, the natural progression of Bicon's design philosophy has resulted in 5.0-mm and 6.0-mm SHORT Implants, which maximize implant placement possibilities and minimize the need for grafting procedures.
Dentsply Sirona's AstraTech family features the OsseoSpeed EV line, with implants available in a versatile range of shapes, diameters, and lengths—6 mm to 17 mm—for all indications, including situations with limited space and/or bone quantity. For conical implants, the body portion is 0.6 mm narrower.
Dentatus' Anew Narrow Body implants are ideal for patients with insufficient bone width, limited interdental space, or converging roots. Designed for use in small interdental spaces for fixed restorations, Anew implants come in diameters of 1.8, 2.2, and 2.4 mm. A nonhygroscopic screw cap allows for implants to be monitored, altered, and easily adapted to a permanent restoration.
For patients whose anatomical limitations prevent them from receiving treatment with standard-diameter implants, the SATURNO Narrow Diameter Implant from Zest Dental Solutions features a 1-piece design with a pivoting O-Ball connection that provides maximum resiliency while maintaining a minimized profile. The implants—available in a straight or a 20° angle for addressing common challenges in the maxillary ridge—come in diameters of 2.0, 2.4, or 2.9 mm and lengths of 10, 12, or 14 mm.
Hiossen Implant's ETIII NH Implant (pictured below and page 66, top) builds on the ET line's sandblasted and acid-etched surface, combined with a bioresorbable apatite nano coating with super hydrophilic properties. These traits include improved boneto-implant contact, increased platelet adhesion, and a more than 30% improvement in osteointegration.
Biocompatibility
In the implant world, titanium—strong, light, nontoxic, and corrosion resistant—has been equated with biocompatibility ever since the first titanium dental implant was placed by Dr. Brånemark in 1965. Now a staple for prosthetic components, zirconia is making inroads for implants as well. It is comparable to titanium in terms of its safety and tissue-friendly nature, but has not been tested long term. Original zirconia implants offered one-piece construction, limiting their flexibility. Two-piece versions will provide greater freedom of placement.
Zimmer Contour Zirconia Abutments from Zimmer Biomet offer a lightcolored base for simple and esthetic all-ceramic restorations that increase patient satisfaction in anterior regions. The strong zirconia material is offered in straight and angled designs and with a variety of cuff heights. They also feature a predefined offset margin that is lower on the buccal and higher on the lingual—virtually eliminating the need to prepare the abutment for a crown.
Digitization
To say that CBCT has revolutionized implant treatment is a huge understatement. This sophisticated 3D-imaging technology has impacted every facet of implantology: diagnostics, surgery and placement, workflow, and productivity. Implant success rates have improved exponentially with the ability to measure every dimension of the implant site, to visualize every feature of the surrounding area from every angle, to design surgical guides, and to monitor integration.
According to Dr. Justin Moody, who operates the Dental Implant Center in Rapid City, SD, CBCT and digital scanning are the 2 essential components required for a successful digital workflow in implant dentistry. With those data sets, he says, clinicians have everything they need to create custom, screw-retained temporaries and healing abutments, as well as the surgical guide. "You can prosthetically plan the implant placement so you know exactly what you need and where it has to go," he shared.
To Come
As research, experimentation, and clinical studies continue, our everyday implant vocabulary will probably expand soon to include 3D printing, zygomatic implants, stem cell therapy, single-visit treatment, and more.
An estimated 5 million implants are placed every year in the United States. With every year that passes, the stellar prognosis improves. The evidence-based reported success rate for single-tooth implants is 98%.
It took centuries to progress from ivory and seashells to stainless steel and titanium. It took decades for standard-size, cylindrical, smooth implants to evolve into customized, threaded, surface-treated implants. It took only a few years for the digital workflow to become standard of care for dental implant therapy. With changes coming at an ever-increasing pace, the future looks bright for dentistry in general, and implantology specifically.
Biocompatibility
In the implant world, titanium—strong, light, nontoxic, and corrosion resistant—has been equated with biocompatibility ever since the first titanium dental implant was placed by Dr. Brånemark in 1965. Now a staple for prosthetic components, zirconia is making inroads for implants as well. It is comparable to titanium in terms of its safety and tissue-friendly nature, but has not been tested long term. Original zirconia implants offered one-piece construction, limiting their flexibility. Two-piece versions will provide greater freedom of placement.
Zimmer Contour Zirconia Abutments from Zimmer Biomet offer a lightcolored base for simple and esthetic all-ceramic restorations that increase patient satisfaction in anterior regions. The strong zirconia material is offered in straight and angled designs and with a variety of cuff heights. They also feature a predefined offset margin that is lower on the buccal and higher on the lingual—virtually eliminating the need to prepare the abutment for a crown.
Digitization
To say that CBCT has revolutionized implant treatment is a huge understatement. This sophisticated 3D-imaging technology has impacted every facet of implantology: diagnostics, surgery and placement, workflow, and productivity. Implant success rates have improved exponentially with the ability to measure every dimension of the implant site, to visualize every feature of the surrounding area from every angle, to design surgical guides, and to monitor integration.
According to Dr. Justin Moody, who operates the Dental Implant Center in Rapid City, SD, CBCT and digital scanning are the 2 essential components required for a successful digital workflow in implant dentistry. With those data sets, he says, clinicians have everything they need to create custom, screw-retained temporaries and healing abutments, as well as the surgical guide. "You can prosthetically plan the implant placement so you know exactly what you need and where it has to go," he shared.
To Come
As research, experimentation, and clinical studies continue, our everyday implant vocabulary will probably expand soon to include 3D printing, zygomatic implants, stem cell therapy, single-visit treatment, and more.
An estimated 5 million implants are placed every year in the United States. With every year that passes, the stellar prognosis improves. The evidence-based reported success rate for single-tooth implants is 98%.
It took centuries to progress from ivory and seashells to stainless steel and titanium. It took decades for standard-size, cylindrical, smooth implants to evolve into customized, threaded, surface-treated implants. It took only a few years for the digital workflow to become standard of care for dental implant therapy. With changes coming at an ever-increasing pace, the future looks bright for dentistry in general, and implantology specifically.
ANCIENT IMPLANTS
Thanks to Dr. Brånemark’s accidental discovery that titanium fuses to bone, the implant landscape is currently at its peak. Materials like zirconia, which exhibit similar properties to titanium, are gaining popularity for their esthetic appeal that more closely resembles a bright tooth color.
But it wasn’t always that way. Ancient times called for creativity in dentistry, and while a few of these “implants” may have been placed postmortem, it doesn’t make the choices any less questionable or intriguing.
Case in PointThanks to Dr. Brånemark’s accidental discovery that titanium fuses to bone, the implant landscape is currently at its peak. Materials like zirconia, which exhibit similar properties to titanium, are gaining popularity for their esthetic appeal that more closely resembles a bright tooth color.
But it wasn’t always that way. Ancient times called for creativity in dentistry, and while a few of these “implants” may have been placed postmortem, it doesn’t make the choices any less questionable or intriguing.

While excavating Mayan ruins in Honduras in 1931, Dr. and Mrs. Wilson Popenoe found 3 carved tooth-shaped shells in the lower jaw of a body. Amazingly, the bone structure around the shell showed signs of regeneration!

Dr. Adam Koppelman